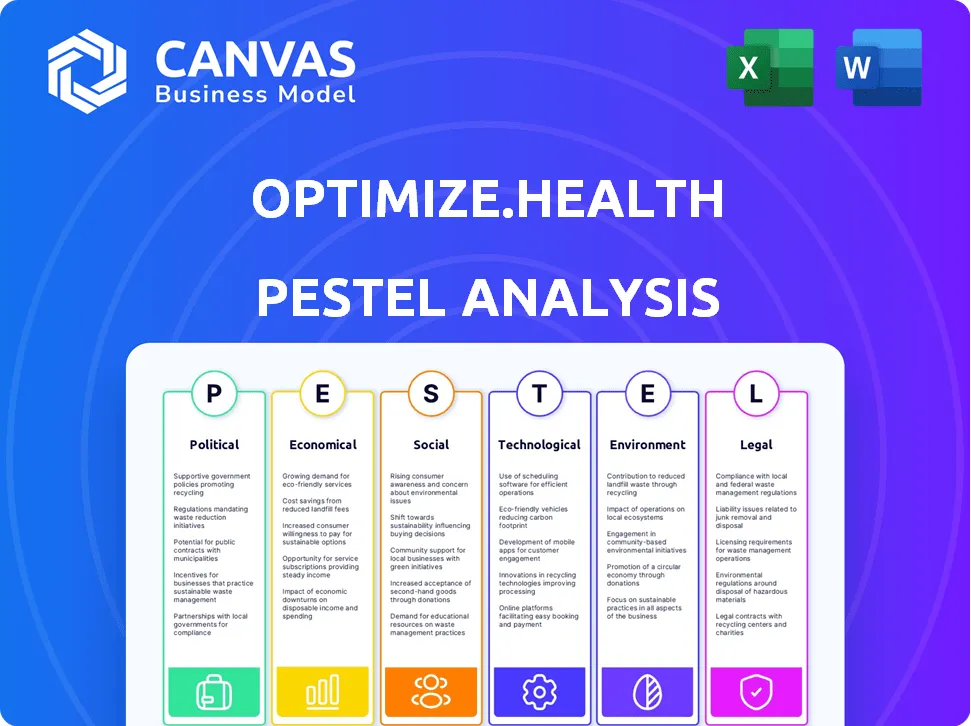
In an era where digital health is becoming the norm, understanding the Political, Economic, Sociological, Technological, Legal, and Environmental (PESTLE) factors that influence companies like Optimize.health is crucial. This innovative platform not only facilitates Remote Patient Monitoring (RPM) but also navigates a complex web of regulations, market dynamics, and societal shifts. Dive deeper below to explore how these interconnected dimensions shape the landscape of digital healthcare, paving the way for enhanced patient outcomes and streamlined care delivery.
PESTLE Analysis: Political factors
Supportive government policies for telehealth.
The COVID-19 pandemic has led to significant policy changes aimed at supporting telehealth services. According to the Centers for Medicare & Medicaid Services (CMS), telehealth utilization increased by over 63% from 2019 to 2020. In 2022, CMS proposed a budget of $4.7 billion for telehealth services.
Regulations promoting Remote Patient Monitoring (RPM).
RPM regulations have been shaped by several federal and state initiatives. As of 2023, the Federal Communications Commission (FCC) allocated $100 million to increase telehealth access as part of the COVID-19 Telehealth Program. The Centers for Medicare & Medicaid Services (CMS) expanded RPM reimbursement policies, allowing an average payment of $51 per patient per month for RPM services.
Funding for digital health initiatives.
Investment in digital health reached a record $29.1 billion globally in 2021, with a significant portion directed towards RPM. In 2022, the National Institute of Health (NIH) announced funding of $10.5 million specifically for remote health technologies. The Health Resources and Services Administration (HRSA) also provided $22 million to improve healthcare delivery through digital platforms.
Potential for changes in healthcare legislation.
Proposals to reform healthcare legislation include expanding access to RPM and telehealth services. As of 2023, the Biden Administration signaled potential enhancements to telehealth policies, with legislative initiatives estimating costs over $5.3 billion for extended telehealth services through 2026.
Influence of political stability on healthcare infrastructure.
Political stability is vital for the growth of healthcare infrastructures. Countries with robust political frameworks, such as Canada and Germany, have seen telehealth adoption rates nearing 70% in 2021. In contrast, instability can detrimentally affect healthcare access, as observed in regions with ongoing conflicts, where healthcare infrastructure typically suffers significantly.
| Factor | Value/Impact |
|---|---|
| Increase in Telehealth Utilization (2019-2020) | 63% |
| CMS Proposed Budget for Telehealth (2022) | $4.7 billion |
| FCC Telehealth Program Allocation | $100 million |
| Average RPM Payment per Patient (CMS) | $51 |
| Global Investment in Digital Health (2021) | $29.1 billion |
| NIH Funding for Remote Health Technologies (2022) | $10.5 million |
| HRSA Funding for Digital Health | $22 million |
| Estimated Costs for Telehealth Policy Enhancements (2026) | $5.3 billion |
| Telehealth Adoption Rate (Canada, Germany) | 70% |
[cbm_pestel_top]
PESTLE Analysis: Economic factors
Growing demand for cost-effective healthcare solutions.
In 2021, the global healthcare market was valued at approximately $8.45 trillion and is expected to grow to $11.9 trillion by 2027, driven by the increasing demand for cost-effective solutions. Consumers and providers are looking for ways to reduce costs while maintaining quality care, which has led to a greater adoption of technologies such as Remote Patient Monitoring (RPM).
Expansion of the digital health market.
The digital health market was valued at $175 billion in 2021 and is projected to reach $660 billion by 2028, growing at a CAGR of approximately 21%. This expansion is driven by increased smartphone penetration, internet accessibility, and a growing preference for telehealth services, especially in the wake of the COVID-19 pandemic.
| Year | Digital Health Market Value (in billions) | CAGR (%) |
|---|---|---|
| 2021 | $175 | - |
| 2022 | $220 (Estimation) | - |
| 2023 | $270 (Estimation) | - |
| 2028 | $660 | 21% |
Economic challenges affecting healthcare budgets.
Healthcare budgets are facing significant pressure, with U.S. healthcare expenditure projected to reach $6.2 trillion by 2028. This escalation is partly due to the aging population and rising incidence of chronic diseases. Hospitals and health systems are being compelled to find innovative ways to manage costs while improving patient outcomes.
Potential return on investment for RPM programs.
Investing in Remote Patient Monitoring programs can yield significant financial benefits. Studies indicate that RPM can reduce hospital readmissions by up to 30% and lower healthcare costs associated with chronic diseases by approximately $5,700 per patient annually. Moreover, for every dollar spent on RPM, there is a potential return of $4.67 in healthcare savings.
| Metric | Value |
|---|---|
| Reduction in Hospital Readmissions | Up to 30% |
| Average Annual Savings per Patient | $5,700 |
| ROI for every $1 spent on RPM | $4.67 |
Increased competition in digital health sector.
The digital health sector is witnessing rapid growth, with over 14,000 digital health companies estimated globally as of 2022. This increasing number of players enhances competition, requiring companies like Optimize.health to innovate continuously to maintain their market position. Investments in technology, marketing, and customer experience are pivotal for sustaining competitive advantage in this dynamic environment.
- Total Number of Digital Health Companies: 14,000
- Estimated Global Funding in Digital Health (2021): $21.6 billion
- Number of Acquisitions in Digital Health (2022): 187
PESTLE Analysis: Social factors
Sociological
Rising patient acceptance of digital health technologies.
The shift towards digital health technology has been noted in various studies, indicating an increase in patient acceptance. According to a survey conducted by the Pew Research Center, 70% of U.S. adults reported they would be interested in using digital health tools, which is an increase of 15% from the previous year.
Emphasis on remote care and convenience.
The convenience factor has significantly influenced patient preferences. A survey by Accenture found that 64% of patients prefer virtual appointments to in-person visits. Furthermore, the global telemedicine market size was valued at approximately $45 billion in 2019, with projections to reach $175 billion by 2026, reflecting a strong emphasis on remote care.
Aging population driving demand for RPM.
The aging population is a critical factor for Remote Patient Monitoring (RPM) services. According to the U.S. Census Bureau, it is projected that by 2030, approximately 20% of the U.S. population will be aged 65 and older. This demographic shift is expected to drive demand for RPM solutions, particularly for managing chronic diseases.
Health literacy impacting technology adoption.
Health literacy plays a crucial role in the adoption of digital health technologies. A report by the National Assessment of Adult Literacy found that only 12% of adults in the U.S. have proficient health literacy skills. This gap may limit the effective use of technologies such as RPM platforms. In contrast, areas with higher health literacy levels show a 40% increase in the usage of digital health tools.
Societal shift towards preventive care models.
The healthcare industry has seen a societal shift towards preventive care. According to the Centers for Disease Control and Prevention (CDC), an estimated $2.6 trillion could be saved in healthcare costs if the U.S. shifts from a reactive to a preventive care model. This shift encourages the adoption of RPM programs which can monitor patients' health continuously to prevent complications.
| Factor | Statistic | Source |
|---|---|---|
| Patient interest in digital health tools | 70% | Pew Research Center |
| Patients preferring virtual appointments | 64% | Accenture |
| Global telemedicine market value in 2019 | $45 billion | Market Research Reports |
| Projected telemedicine market value by 2026 | $175 billion | Market Research Reports |
| U.S. population aged 65 or older by 2030 | 20% | U.S. Census Bureau |
| Adults with proficient health literacy | 12% | National Assessment of Adult Literacy |
| Increased usage of digital health tools with high health literacy | 40% | Health Literacy Studies |
| Estimated savings from preventive care shift | $2.6 trillion | Centers for Disease Control and Prevention (CDC) |
PESTLE Analysis: Technological factors
Advancements in telehealth technology
The telehealth market has seen significant growth, with a projected market size of $459.8 billion by 2030, growing at a CAGR of 22.4% from 2022 to 2030. The COVID-19 pandemic accelerated the adoption of telehealth, with a 38% increase in telehealth visits recorded in 2020.
Integration of AI and machine learning in RPM
The AI healthcare market is expected to reach $188 billion by 2030, with machine learning playing a pivotal role. Companies integrating AI in their RPM solutions have reported improvements in patient outcomes by up to 30% through predictive analytics and personalized care.
Increased use of wearable health devices
The global wearable medical devices market is anticipated to grow from $28.3 billion in 2022 to $173 billion by 2030, at a CAGR of 26.8%. Devices like smartwatches and fitness trackers are increasingly used in RPM programs, with 64% of healthcare providers reporting the integration of wearables to monitor patient health remotely.
| Year | Market Size (USD Billion) | CAGR (%) |
|---|---|---|
| 2022 | 28.3 | N/A |
| 2030 | 173 | 26.8 |
Importance of data security and privacy technologies
With the increase in digital health solutions, the global healthcare cybersecurity market is projected to reach $66.8 billion by 2027, up from $18.6 billion in 2020. Following the implementation of the Health Insurance Portability and Accountability Act (HIPAA) regulations, non-compliance costs averaged around $1.5 million per incident, emphasizing the critical nature of security in telehealth.
Need for seamless integration with existing health systems
According to a survey conducted by the Healthcare Information and Management Systems Society (HIMSS), approximately 74% of healthcare leaders indicated that interoperability and seamless integration are top priorities for their organizations. The cost of disconnected health systems has been estimated at around $250 billion annually in the United States due to inefficiencies.
PESTLE Analysis: Legal factors
Compliance with healthcare regulations (e.g., HIPAA)
Optimize.health operates in a highly regulated environment, particularly adhering to the Health Insurance Portability and Accountability Act (HIPAA). In 2020, the Department of Health and Human Services (HHS) reported that 30% of healthcare organizations faced significant compliance challenges due to the complexity of regulations.
Non-compliance can result in fines ranging from $100 to $50,000 per violation, depending on the level of negligence, with a maximum penalty of $1.5 million per year.
Intellectual property considerations in digital health
The digital health space is increasingly competitive, and Optimize.health must protect its intellectual property vigorously. In 2021, investment in digital health startups reached approximately $29.1 billion, underscoring the importance of patent protection for proprietary technologies.
As of 2022, there were around 7,500 active digital health patents in the United States, making it critical for companies to secure their IP to maintain a competitive edge.
Liability issues related to RPM data
Legal liabilities arise primarily from data breaches and inaccuracies in Remote Patient Monitoring data. According to the 2021 Verizon Data Breach Investigations Report, healthcare was the most targeted sector, accounting for 79% of data breaches. The financial impact of a single data breach can reach up to $3.86 million.
Additionally, the risks associated with incorrect RPM data can lead to misdiagnosis or delayed treatments, which can result in malpractice claims averaging between $15,000 to $50,000 in legal costs per incident.
Changes in laws affecting telemedicine practice
In 2021, 38 states in the U.S. enacted temporary policies to enhance telehealth access amid the COVID-19 pandemic, with many of these policies potentially becoming permanent. The rise in telehealth utilization grew by 154% from 2019 to 2020, with telehealth visits reaching 50 million in 2020 alone.
The Centers for Medicare & Medicaid Services (CMS) indicated that telehealth services could incur payment updates, impacting reimbursement rates, which account for 12% of the total healthcare spending estimated at $4 trillion in 2021.
International regulations impacting global operations
Operating internationally exposes Optimize.health to varying regulations. The General Data Protection Regulation (GDPR) in Europe imposes strict data protection requirements, with potential fines up to €20 million or 4% of total annual global turnover, whichever is higher.
As of 2023, there were approximately 1,200 health tech companies operating under international markets, facing different regulatory landscapes that can significantly affect their operations, particularly in the EU and Asia.
| Aspect | Details | Data/Statistics |
|---|---|---|
| HIPAA Compliance Fine Range | Minimum to Maximum Penalty | $100 to $50,000 per violation; up to $1.5 million per year |
| Digital Health Patent Activity | Active Patents | 7,500 active patents in the U.S. (as of 2022) |
| Average Data Breach Cost | Healthcare Sector | $3.86 million per breach (2021) |
| Malpractice Claim Costs | Legal Cost per Incident | $15,000 to $50,000 |
| Telehealth Growth Rate | Increase in Utilization | 154% increase from 2019 to 2020 |
| Healthcare Spending (U.S.) | Total Estimated | $4 trillion in 2021 |
| GDPR Fines | Maximum Possible Financial Penalty | €20 million or 4% of annual global turnover |
PESTLE Analysis: Environmental factors
Focus on sustainable healthcare practices
As of 2022, the healthcare sector accounted for approximately 8.5% of the total greenhouse gas emissions in the United States, highlighting the urgent need for sustainable practices. Initiatives to reduce this environmental impact are increasingly being adopted by healthcare providers. Optimize.health has actively sought partnerships with organizations aiming to promote sustainability within healthcare delivery.
Impact of technology on carbon footprint
The integration of technology in healthcare presents both advantages and challenges regarding carbon emissions. The shift towards Remote Patient Monitoring (RPM) can potentially reduce hospital visits by 39%, thereby decreasing the overall carbon footprint associated with transportation. According to a report by the Global e-Sustainability Initiative, digital technology in healthcare could reduce global CO2 emissions by up to 1.5 gigatons per year by 2030.
Potential for RPM to reduce healthcare's physical space needs
Implementing RPM significantly decreases the need for physical space in hospitals. A well-structured RPM program can lead to a reduction in hospital bed demand by up to 30%. This could save approximately $4,000 per hospital admission. With healthcare facilities operating at a capacity of around 70%, optimizing physical space utilization becomes a critical element in promoting sustainability.
Regulatory considerations for electronic waste
The healthcare industry is projected to generate 9 million tons of electronic waste by 2025. Regulations such as the Waste Electrical and Electronic Equipment (WEEE) Directive necessitate that companies like Optimize.health adopt responsible electronic waste recycling practices. Compliance costs related to e-waste regulations can amount to $5 billion annually in the United States, making it essential for organizations to integrate these costs into their operational budgets.
Advocacy for eco-friendly digital health solutions
There is a rising demand for eco-friendly digital health solutions. According to a survey conducted by the Health Information Management Systems Society (HIMSS), approximately 70% of healthcare organizations are looking to invest in sustainable IT solutions by 2025. Digital health companies have a unique opportunity to position themselves as leaders in this movement, with a potential market for sustainable healthcare technologies anticipated to reach $70 billion by 2027.
| Factor | Statistic/Impact | Source |
|---|---|---|
| Healthcare Emissions | 8.5% of total U.S. emissions | United States Environmental Protection Agency |
| Reduction in Transport Emissions | 39% decrease in hospital visits | Global e-Sustainability Initiative |
| Potential Reduction in Hospital Beds | 30% reduction in bed demand | Healthcare Institute |
| Electronic Waste Generation | 9 million tons by 2025 | Institute of Scrap Recycling Industries |
| Investment in Sustainable IT | 70% of organizations by 2025 | Health Information Management Systems Society |
| Sustainable Healthcare Market | $70 billion by 2027 | Market Research Report |
In summary, the PESTLE analysis of Optimize.health reveals a dynamic landscape shaped by various interrelated factors. Politically, there is strong support for telehealth initiatives; economically, the demand for cost-effective solutions continues to surge. Sociologically, an aging population and increased health literacy are driving acceptance of digital health technologies. Furthermore, technological advancements, particularly in AI and wearables, enhance the effectiveness of Remote Patient Monitoring. Legally, compliance issues must be navigated cautiously, while environmentally, there is a growing emphasis on sustainability within healthcare practices. By understanding these critical dimensions, Optimize.health can strategically position itself to thrive in the rapidly evolving digital health sector.
[cbm_pestel_bottom]

![Erol Alkan - Reworks Volume 1 Boxset [PHLP08X] Erol Alkan - Reworks Volume 1 Boxset [PHLP08X]](https://www.watchcharm.shop/image/erol-alkan-reworks-volume-1-boxset-phlp08x_eSXmRV_300x.webp)